
The patient's ability to tolerate surgery without significant morbidity is an important factor in triaging advanced epithelial ovarian cancer (AEOC) patients for initial surgical management

Vizzielli’s Score Calculator

What is it about?
The patient's ability to tolerate surgery without significant morbidity is an important factor in triaging advanced epithelial ovarian cancer (AEOC) patients for initial surgical management. Indeed, the clinician could use this information to personalize decisions regarding upfront surgical cytoreduction versus neoadjuvant chemotherapy. The aim of our model is to develop and validate a simple adjusted laparoscopic score to predict major postoperative complications after primary debulking surgery (PDS) in AEOC.
App Store Description
The patient's ability to tolerate surgery without significant morbidity is an important factor in triaging advanced epithelial ovarian cancer (AEOC) patients for initial surgical management. Indeed, the clinician could use this information to personalize decisions regarding upfront surgical cytoreduction versus neoadjuvant chemotherapy. The aim of our model is to develop and validate a simple adjusted laparoscopic score to predict major postoperative complications after primary debulking surgery (PDS) in AEOC.
To obtain a simple and easily applicable pre-operative score, the number of potential predictors
was a priori restricted to the parameters with the best performance (p less than 0.2) at multivariate analysis. Overlapping factors were removed based on their strong correlation and subsequent overfitting risk. The study population was randomly divided in a “derivation group” (n = 370) representing two-thirds of overall patients, and in a “validation group” (n= 185).
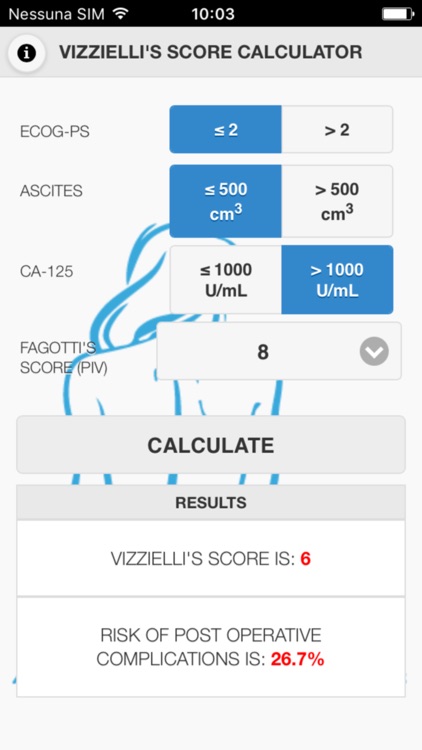
The multivariate model to predict major complications was developed in the derivation group. The regression coefficients of the predictive parameters were shrunk by the calculated constant shrinkage factor (0.94) and then transformed the results into simple points. The mean risk for each point was calculated, and a scale to associate the predicted risk to each score was developed. Significant predictors included in the scoring system were: poor performance status, presence of ascites (N greater than 500 cm3), CA125 serum level (N greater than 1000 U/ml), and high laparoscopic tumor load (predictive index value, PIV=8). The sum of each value for each variable made the overall predictive risk score, which ranged between 0 and 8. Then, the score and the predicted risk were computed for each patient in the validation population, and these new variables were tested using the c-statistic and the Hosmer–Lemeshow test. Since our model was developed and validated on the same data, the performance could be too optimistic. However, to correct for the optimism in discriminative ability, the steps taken into Cox regression were internally validated by 200 random bootstrap samples and a subsequent correction for optimism in the c-statistic was performed. Moreover, since the model reflects a continuum of risk assessment, women were equally categorized a priori into three different classes: high risk group for score between 6 and 8, intermediate risk group for score between 3 and 5, and low risk group for score between 0 and 2. The prediction of risk of major complications using the score as progressive values is:
2.2% for score 0
3.5% for score 1
5.4% for score 2
8.4% for score 3
12.7% for score 4
18.7% for score 5
26.7% for score 6
36.7% for score 7
47.9% for score 8
The mean risk of developing major postoperative complications was 3.7%, 13.2% and 37.1% for low risk group, intermediate risk group and high risk group, respectively.
To make more user-friendly this model, we have thought to develop an application for mobile devices. Indeed, despite the accuracy of internal validation by using a randomly selected 33% of the study cohort, a limitation of our model is the lack of validation in other centers and healthcare systems, which is a prerequisite for large-scale adoption of this score. In this context, although we acknowledge that laparoscopy is not adopted in many international centers, our results increase its indications and call for a larger use as valuable diagnostic tool in AEOC. Moreover, this application for mobile devices increase its reproducibility. Lastly, through this app, the surgeon may accurately and easily predict a patient's postoperative outcome with an early identification of high-risk woman, thus adopting tailored strategies on individual basis.
* Vizzielli G, et al. A laparoscopic risk-adjusted model to predict major complications after primary debulking surgery in ovarian cancer: A single-institution assessment. Gynec Oncol. 2016 Jul;142(1):19-24.
AppAdvice does not own this application and only provides images and links contained in the iTunes Search API, to help our users find the best apps to download. If you are the developer of this app and would like your information removed, please send a request to takedown@appadvice.com and your information will be removed.